I worked on rare genetic diseases during my PhD and looked for novel disease causal genes – which I was lucky enough to find1. I also became familiar with the state of rare disease therapeutics: there over 7,000 rare diseases for which only %5 have therapies2. A large majority of rare diseases are neglected by Pharma companies most probably as the market is not as big as it is for common diseases (e.g. obesity, diabetes, COPD). Thus, when I was approached by an old family friend out of the blue and told that his 11 month-old son was a spinal muscular atrophy (SMA) type 1 patient, I straight away thought “the child probably has no hope“.
I did not mention the lack of therapies for rare diseases to my friend and did some research about SMA – a severe neuromuscular disorder where many patients die before the age of two. I was surprised to see that there was an apparently effective ‘cure’: Zolgensma, a gene therapy/drug that Novartis are offering for ~$2.1 million – the world’s most expensive drug at present. Although the drug is FDA and EMA approved, the NHS does not offer the drug at the moment as it has not been reviewed by the NICE committee – which thoroughly reviews all credible drugs and advises the NHS on whether to offer it to UK patients or not.
As we saw that quite a few parents ran successful crowdfunding campaigns and got their children to have the therapy, we decided to do the same (Metehan’s Gofundme page). As the crowdfunding campaign gathered pace, I was sent a tonne of emails – including the academics listed below – asking how Novartis can charge such a price for one drug. While we understand that this is not just a quest for profits and the price reflects R&D and production costs as well as Zolgensma’s position compared to competitors such as Spinraza (Biogen) – offered by the NHS, which is thought to cost around ~£400,000 per patient (real price unknown due to undisclosed agreement3) for just the first year – we believe that Novartis should provide a breakdown of what the profit margin of Zolgensma is per patient.
While we commend Novartis and other companies for investing in rare diseases and can only hope more would follow suit, disclosing profit margins would be most ethical thing to do, which in turn can provide a room for negotiation for patients, and low and middle-income countries (LMIC).
Dr A. Mesut Erzurumluoglu, Research Associate/Genetic Epidemiologist (MRC Epidemiology Unit, University of Cambridge)
Signed by:
Dr Zeynep Hulya Gumus, Assistant Professor of Genetics and Genomic Sciences (Icahn School of Medicine, Dept. of Genetics and Genomics)
Dr Sevinc Ercan, Associate Professor of Biology (New York University, Faculty Director of Diversity, Equity and Inclusion)
Prof. Cem Say, Professor of Computer Science (Bogazici University, Dept. of Computer Science)
Short link to share this call: bit.ly/smanovartis
References
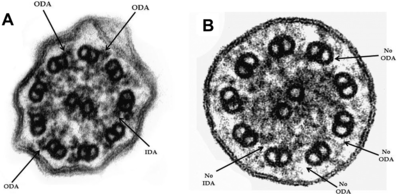
- Alsaadi, M.M. and Erzurumluoglu A.M. et al. Nonsense mutation in coiled-coil domain containing 151 gene (CCDC151) causes primary ciliary dyskinesia. Human Mutation 35, 1446-8 (2014). (Also see my blog post: Discovery of a new Primary ciliary dyskinesia causal gene)
- Tambuyzer, E. et al. Therapies for rare diseases: therapeutic modalities, progress and challenges ahead. Nature Reviews Drug Discovery 19, 93-111 (2020).
- National Institute For Health And Care Excellence – Final appraisal document: Nusinersen for treating spinal muscular atrophy. July 2019. URL: https://www.nice.org.uk/guidance/ta588/documents/final-appraisal-determination-document-2. Accessed: 10/09/2020